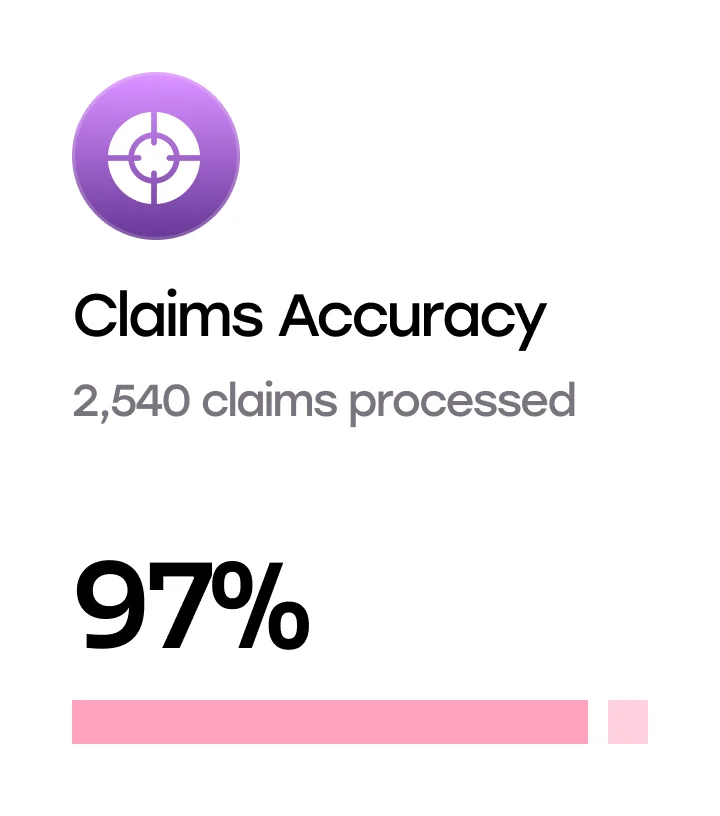
Lower Claims Management Cost.
Drive Operational Efficiency With SHAI
Streamline Claims Processing
Accelerate the claims lifecycle, drive accuracy, and reduce errors.
Coding Expertise to Spot Errors Pre-Submission
Post-Payment Claims Audit
Claim Adjudication
Claims Adjustments
Appeals and Grievances Processing
Multi-Domain Claims Processing (Pharmacy, Dental, Vision, etc)

Accelerate Benefits
and Enrollment Processing
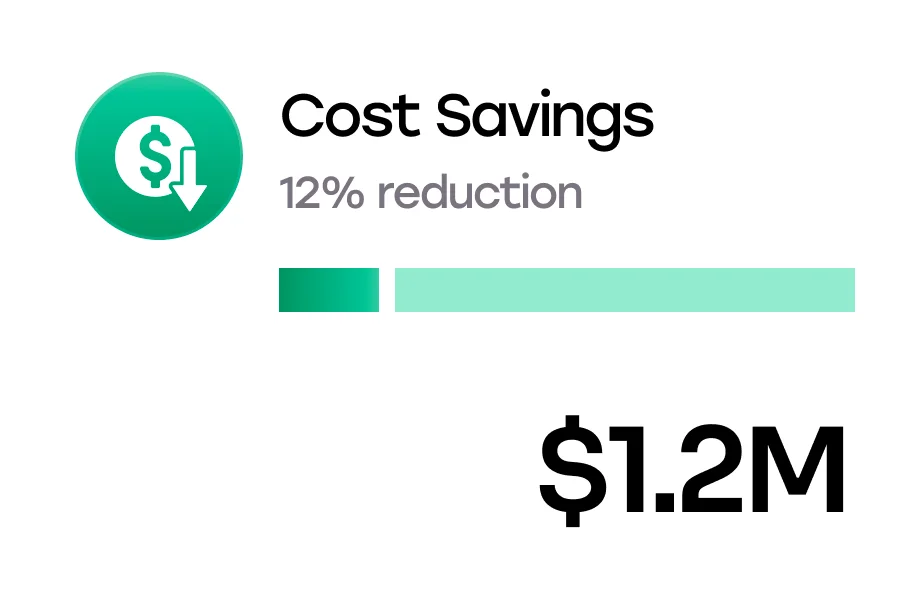
Enhance member experience and efficiency through tailored processing and maintenance across the member-payer relationship.
Benefits Configuration and Testing
Medicare, Medicaid, ACA, and payment reconciliation
Member Enrollment & Reconciliation
Premium Billing and Invoicing Services

Manage Provider Data End-to-End
Maintain, update, and analyze provider network data to reduce admin work in loading data, improve network data accuracy, and adhere to compliance regulations.
Provider Intake
Credentialing
Provider Data Aggregation and Validation
Compliance Insights
Contract Configuration and Modeling
Testing

Mitigate Risk With Quality Assurance
Run risk adjustment programs spanning multiple plans, states, and technological changes, improve risk scores, and meet compliance regulations with 360* data collection.
Chase List and Retrieval
Risk Score Chart Review
HEDIS Chart Follow-ups And Review
Documentation and Data Collection For Compliance
Manage Benefits Utilization
Review cases. Assess medical appropriateness with data-driven techniques. Lower healthcare cost.
Prior Auth Intake
Case Management
Prospective, Concurrent, and Retrospective Planning and Review
Disease Management
How SHAI Handles Transitions and Quality Assurance

Refresher Sessions and 1:1 Training
Weekly EBTs (Error-Based Trainings) and PKTs (Process Knowledge Tests)
RCA, 5 Whys, Fishbone Analysis, Pareto Chart, and CAPA (Corrective Action Preventive Action)
Proactive Daily Team Huddles With Peer Audits
Periodic Calibrations For Continuous Improvement
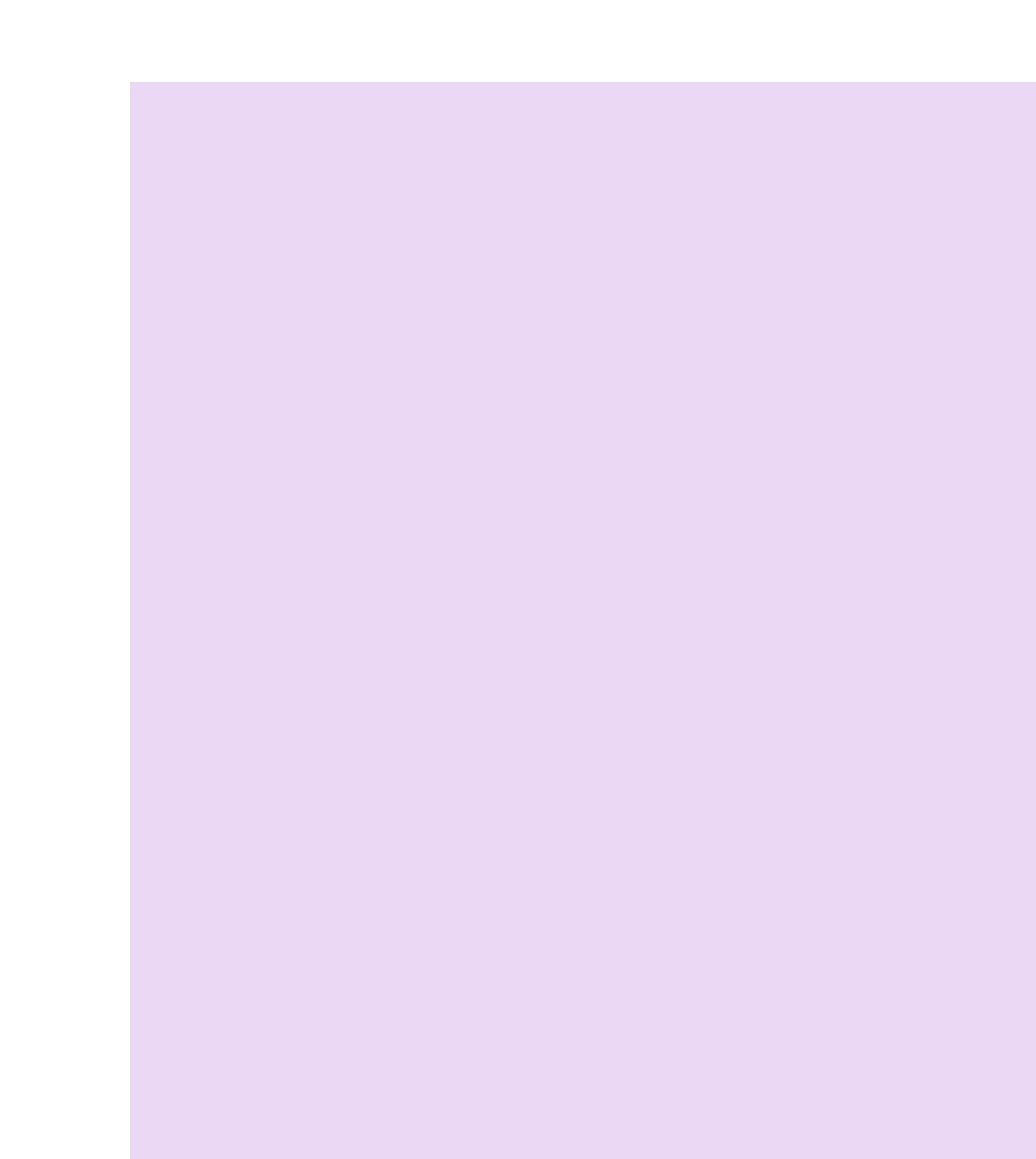
The Numbers Speak For Themselves
98%+
Transaction Accuracy
40-60%
Payroll Cost Reduction
98%
Financial Accuracy
<5%
AR Time Reduction
20%+
Increase in Collections
99%+
Vendor SLA Compliance
<2%
Denial Rate
90%+
Increase in First Pass Rate
95%+
Claims Adjudicated Within 30 days
Secure. Compliant.
A Payer Services Provider You Can Trust.

ISO 27001
![HIPAA ,[object Object], compliant](/_next/image?url=%2Fimages%2Fhome%2FsecureSectionImg2.webp&w=256&q=75)
HIPAA
compliant
![PHI Policy Rigor With ,[object Object], Clean Desk Policy](/_next/image?url=%2Fimages%2Fhome%2FsecureSectionImg3.webp&w=256&q=75)
PHI Policy Rigor With
Clean Desk Policy
![Purpose-Built SSO ,[object Object], Login and Cloud Infra](/_next/image?url=%2Fimages%2Fhome%2FsecureSectionImg4.webp&w=256&q=75)
Purpose-Built SSO
Login and Cloud Infra
The SHAI Promise
Not just a Payer Services provider, but a reliable business partner who works continuously to drive growth & operational efficiency through talent & tech-solutions
STEP 01
Payer Process Audit
STEP 02
Gap Analysis
STEP 03
Solutioning Scope with 24-48 Hours TAT
STEP 04
Systematic Monitoring and Feedback Loop